- Prescription opioid misuse has become a growing public health concern in the UK and dihydrocodeine addiction is a fast-growing problem.
- Dihydrocodeine is the most commonly prescribed opioid for treating moderate to severe pain in the UK.
- It is often used to treat arthritis, post-operation pain and chronic injuries. In recent times, the use of opioids (including dihydrocodeine) has rapidly increased by a variety of means including bona fide prescription and illicit use.
Prescription opioid misuse has become a growing public health concern in the UK and dihydrocodeine addiction is a fast-growing problem. Primarily used to treat moderate to severe pain, dihydrocodeine leads to physical and psychological dependence, more so with long-term use.
Dihydrocodeine is one of the more commonly misused drugs, as data shows that opioid prescriptions and addiction rates have risen recently in the NHS.
Dihydrocodeine is the most commonly prescribed opioid for treating moderate to severe pain in the UK. It is often used to treat arthritis, post-operation pain and chronic injuries.
In recent times, the use of opioids (including dihydrocodeine) has rapidly increased by a variety of means including bona fide prescription and illicit use. This follows the same trend as a growing global alarm over the use of opioids, which has been called an epidemic in the US and Canada, among many other countries.
It’s no different in the UK, where the discussion around addiction and substance abuse is becoming more common, and prescription opioids like dihydrocodeine are making their way into the conversation.
The case with dihydrocodeine in particular is problematic because it is very addictive. Like many other opioids, it works on the brain to decrease pain and produce feelings of euphoria. Repeated use of the drug can result in a euphoric effect, which can cause individuals to misuse the drug in an attempt to re-experience the feeling of relief or pleasure.
It begins a legitimate medical treatment, quickly becomes a dependence, and then an addiction. In the UK, dihydrocodeine is the only prescription opioid available, and cases of addiction have shot up because of it. The usual legal over-the-counter dose is less than 8mg [1].
Many people begin with low-dose pain relief prescriptions but go on to misuse their medication by taking more than they were prescribed or using the drug recreationally. The pattern has been a contributory factor to rising cases of addiction and an increased number of drug-related deaths, including overdoses involving opioids.
What Is Dihydrocodeine: Medical Uses And Prescriptions
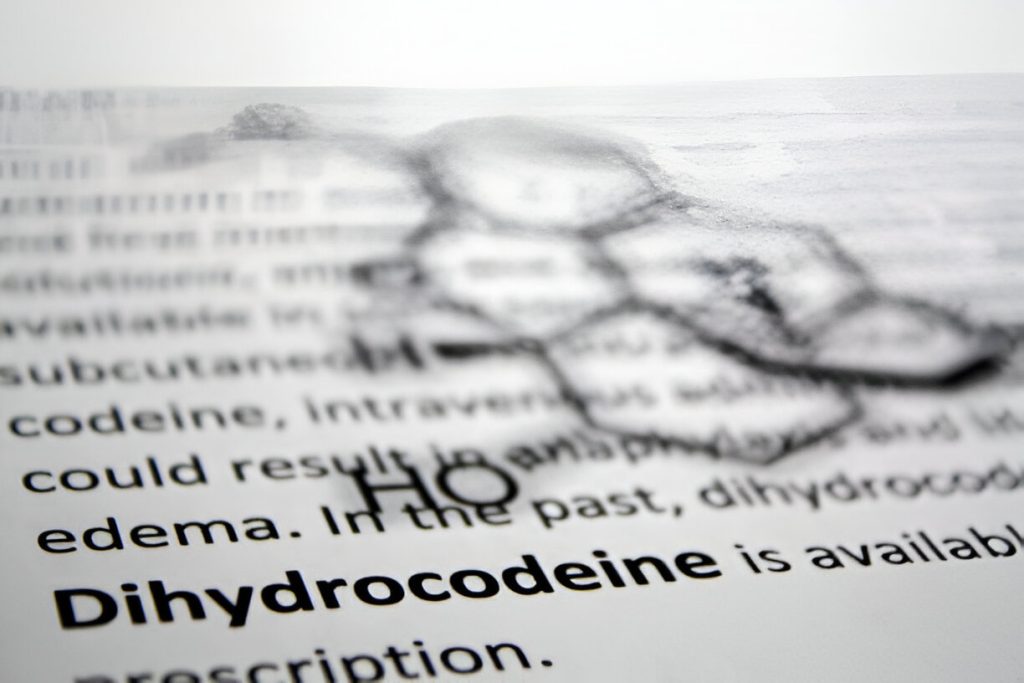
Dihydrocodeine is a semi-synthetic opioid created from codeine. According to Cancer Research UK, it is available in different forms, such as tablets, capsules and liquid formulations, and is usually prescribed to manage moderate to severe pain.
Dihydrocodeine is usually prescribed in medical settings when over-the-counter pain relievers, such as paracetamol or ibuprofen, do not control a patient’s pain. For example, dihydrocodeine is used in the UK as part of pain management strategies for chronic conditions (e.g. severe arthritis or cancer pain) so it is important for many patients.
Why Is Dihydrocodeine Addictive
Dihydrocodeine has addiction potential. The drug binds to opioid receptors in the brain, changing how the brain perceives pain and prompting the release of a neurotransmitter called dopamine — which is linked to a feelgood high [2]. In the long run, users can build a tolerance, meaning they need more of the drug to create the same response.
The pattern of ever-increasing dosage can cause dependence, where the body becomes dependent on the drug to function properly, and then addiction, where the users become unable to function properly without it, and will compulsively seek out the drug, regardless of the negative consequences.
Dihydrocodeine’s addictive potential is particularly worrying because people may not realise the risks when they start taking it. The patient taking the medication for pain relief will follow the doctor’s instructions but will develop a dependence on the drug over time. You go through withdrawal symptoms that make it harder to avoid dependence after you start.
How Dihydrocodeine 30mg Pills Are Misused Recreationally In The UK
Dihydrocodeine 30mg pills have a reputation for recreational misuse in the UK. A lot of people get these pills via prescription fraud, buying them off the black market or taking them inappropriately with a legitimate prescription [3]. The euphoric “high” that recreational users chase — that big hit — can mimic the effects of stronger opioids such as morphine or heroin. Using dihydrocodeine in this way is very dangerous as it greatly increases the risk of overdose and long-term addiction.
Dihydrocodeine And Alcohol: The Risk Of Mixing Substances
One of the particularly dangerous practices related to the recreational use of dihydrocodeine is mixing it with alcohol. Dihydrocodeine and alcohol are depressants; they slow the central nervous system. In combination, they may cause profound sedation, respiratory depression and death. Together they are particularly deadly because they can dampen the body’s natural urge to breathe, making overdose occur faster than if the drug is taken alone.
How Long Does Dihydrocodeine Stay In Your System
Depending on the dose and how quickly that individual processes the dihydrocodeine, the effects usually last four to six hours. But like other opioids, it’s addictive because users can experience a ‘crash’ as the drug wears off, and they take more to prevent withdrawal symptoms or to keep the high.
The continual cycle of use and withdrawal common in addiction is a primary source of addiction since it can instigate compulsive drug-seeking behavior and rising doses.
Like other opioids, dihydrocodeine, when taken as prescribed, can bring about several side effects. Common physical side effects include [3]:
- Drowsiness and dizziness
- Nausea and vomiting
- Typical opioid side effect: constipation.
- Headaches
- Dry mouth
These side effects can get worse in some cases — especially when the drug is taken as a misused drug or in high doses. Dihydrocodeine is sedative and people often have trouble functioning normally because of it, and it interferes with work, social activities and daily responsibilities.
Dihydrocodeine 30mg Pill Side Effects: What You Need to Know
The most commonly misused form of the drug in the UK is dihydrocodeine 30mg pills. The side effects are much more severe when the drug is taken recreationally or in doses above the prescribed dose.
These include:
- Respiratory depression (slow and shallow breathing)
- Extreme drowsiness and confusion
- In severe cases, loss of consciousness or coma may occur.
- Overdose when taken with other depressants such as alcohol, sedatives
The drug also causes mental side effects, particularly when used over a long period. As addiction is a cycle, it can lead to anxiety, depression and mood swings. Opioids become the crutch the brain’s reward system depends on, and when the drug isn’t available, emotional instability results.
Long-Term Impact Of Dihydrocodeine Addiction On Health
Dihydrocodeine addiction has serious long-term consequences on physical and mental health. Prolonged use of dihydrocodeine can damage the liver, kidneys and the digestive system physically. Chronic lung problems can result from the drug’s constant suppression of respiratory function, and the longer a user uses the drug the higher the risk of fatal overdose.
Long-term dihydrocodeine addiction can have a significant impact on mental health [2]. Without the drug, their brain struggles to regulate mood which results in many users developing severe depression and anxiety. It can create a cycle of self-medication, where people will take more of the drug to get rid of the mental health symptoms, just making the addiction worse.
Long-term users can also have cognitive function deteriorate to the point of being unable to focus or remember things, making life more difficult and recovery longer.
How An Overdose Occurs
There are many reasons that people can overdose on dihydrocodeine, usually simply by accident or overuse. An overdose occurs when a person uses too much of the drug, too quickly for the body to be able to process it safely. The biggest threat from an opioid overdose is called respiratory depression when the body stops breathing or slows down breathing. If left untreated quickly, this lack of oxygen can lead to brain damage, coma or death.
Dihydrocodeine is more likely to cause an overdose when used with other depressants, like alcohol benzodiazepines, or some sleeping pills. These substances have a compounding effect on the central nervous system, making it more likely that the patient will succumb to life-threatening respiratory failure.
Symptoms Of Overdose And What To Do
Knowing the signs of a dihydrocodeine overdose can help to save lives. Key signs include:
- Extreme drowsiness, or inability to wake up
- Slowed or irregular breathing
- Blue or pale skin, especially around the lips or nails (from lack of oxygen)
- Pinpoint pupils
- Low blood pressure or weak pulse
- Reduced consciousness or inadequate response to stimuli.
When you think someone is having an overdose, it’s important to get them medical help right away. The drug that reverses opioid overdose, naloxone, is becoming more widely available in the UK [2]. In emergencies, it can be administered to reverse opioid effects and buy time until the medical professionals can do their job. But naloxone is not a cure and you should always seek medical help as soon as possible.
What Happens During Dihydrocodeine Withdrawal
Dihydrocodeine withdrawal is when someone dependent on dihydrocodeine abruptly reduces their dose or stops this drug completely. Withdrawal symptoms can be physically and mentally very distressing and most people can’t give up without professional help.
Physical withdrawal symptoms typically begin within a few hours to a day after the last dose and can include:
- Sweating and chills
- Muscle aches and pains
- Nausea, vomiting and diarrhoea.
- Restlessness and insomnia
- Rapid heart rate
Anxiety, irritability and wanting the drug are some of the things that are going on mentally. Just as difficult as the physical ones, these psychological symptoms often push people back into relapse—away from the discomfort they experience.
How To Control Withdrawal Symptoms And Reduce Your Risk Of Relapse
One of the most important things to do in recovery is to manage withdrawal symptoms. In the UK, the safety and well-being of the individual can be maintained when opioid withdrawal is managed under medical supervision. In some cases, substitution therapies, like methadone or buprenorphine are used to help decrease withdrawal symptoms by supplying a controlled, smaller dose of opioids to the body. This can help you get rid of cravings and enable you to slowly get off the drug.
In addition to medical treatment, counseling and therapy are needed to reduce the chance of relapse. People working with cognitive–behavioral therapy (CBT) and other forms of psychological support can find out what triggers and triggers of addiction and how to deal with stress and cravings more healthily.
Available Treatment Programs for Dihydrocodeine Addiction
Dihydrocodeine addiction can be treated with many different programmes in the UK. They can be anything from community-based support groups to residential rehab centres. The treatment you choose will depend on your addiction severity, your health and personal preferences.
Detox Programs: The first step in treating dihydrocodeine addiction is usually detox. Detox is a process whereby an individual is medically supervised as they safely withdraw from the drug during detox. Methadone or buprenorphine can be given by detox centres in the UK to help the withdrawal symptoms when coming off dihydrocodeine, lessening the misery associated with kicking the habit.
Inpatient Rehab Centres: Those with more severe addictions may benefit from a structured environment outside of their everyday triggers, in a residential treatment center. Patients get 24-hour medical care, therapy and support from professionals who specialize in opioid addiction in these settings. Usually, these programs last 28 days to several months, depending on the client’s needs.
Outpatient Treatment: Outpatient programs provide treatment sessions scheduled at a particular time and place, allowing individuals to live at home while being treated. This is for people with milder addiction or people who have to take care of work or family. Therapy, counseling and medication-assisted treatment (MAT) are the usual treatments for outpatient treatment.
Support Groups: There are support groups such as Narcotics Anonymous that provide support to people recovering from opioid addiction. Secondly, these groups are a safe space in which people can share their experiences supporting each other through the recovery process. Support groups are another way that help people cope with problems while being ‘an adjunct to formal treatment programs.’
Overcoming Addiction: From Detox To Long-Term Recovery In The UK
Detox is not the end point in overcoming dihydrocodeine addiction. Recovery is a long-term process and involves a combination of ongoing therapy, changes to lifestyle, and professionals and loved ones to support you. Aftercare programs are essential in the UK to help people stay on track once their initial treatment is completed.
Therapy and Counseling: The most effective form of addiction treatment therapy is Cognitive Behavioral Therapy (CBT). It helps people to find out which negative thought patterns and behaviours contribute to their addiction and how to develop healthier behaviours when dealing with stress or boredom. Other approaches to therapy include group therapy, family therapy, and mindfulness-based practices, which may all be incorporated into a wide range of treatment plans.
Medication-Assisted Treatment (MAT): In some instances, MAT continues after detox to prevent relapse. An addiction treatment works by using medications such as methadone or buprenorphine delivered on a controlled basis to help treat cravings and withdrawal symptoms. When MAT is used, it is often used in combination with therapy and counseling to treat the whole person.
Relapse Prevention: Preventing relapse is one of the biggest obstacles in recovery. A good relapse prevention plan is encouraged to be made by individuals who learn to identify triggers, avoid high-risk situations, and stay connected to a strong support network. In the UK however, many treatment centres have aftercare services available which offer continued support from counselors and support groups after an individual completes his initial treatment program.
Ongoing Support Is Essential
Addiction is often a chronic condition — one that needs to be managed on an ongoing basis for many people. In the UK the importance of continued support after treatment is paramount. For instance, it could include contacting a therapist daily, going to support group meetings, or maintaining contact with a sponsor. There are many different types of continuing care available from the National Health Service (NHS) and charities around the UK to assist people to remain sober and reintegrate into society after treatment.
1. Wikipedia. Dihydrocodeine. https://en.wikipedia.org/wiki/Dihydrocodeine
2. NHS. Common questions about dihydrocodeine. https://www.nhs.uk/medicines/dihydrocodeine/common-questions-about-dihydrocodeine/
3. Health Direct. Dihydrocodeine. https://www.healthdirect.gov.au/dihydrocodeine
The Article
About This Article
✔ Medically Reviewed
✔ Evidence-Based Sources
✔ Updated Regularly
✔ Clinically Verified
This article was written by THE BALANCE’s clinical content team and reviewed by a licensed medical or mental health professional (such as an MD, psychiatrist, clinical psychologist, or equivalent). Our reviewers ensure that the information reflects current research, accepted medical guidelines, and best practices in mental health and addiction treatment. THE BALANCE’s medical editors draw on extensive real-world clinical experience supporting individuals in residential, outpatient, and luxury private treatment settings across Europe and internationally.
Editorial Standards & Integrity
THE BALANCE follows strict editorial and clinical review standards to ensure accuracy, balance, and reliability:
- All medical statements rely on authoritative sources such as the WHO, NIMH, APA, NHS, CDC, and SAMHSA
- Statistics use the most recent and reliable research available
- No medical or therapeutic claims are made without clear, verifiable evidence
- Content is reviewed and updated regularly to reflect evolving science, treatment guidelines, and clinical best practices
- Commercial interests do not influence clinical accuracy; all clinical insights are reviewed independently
- Recommendations include context, limitations, and alternatives where appropriate
How We Review Sources
- Our clinical writers and editors rely on:
- Peer-reviewed research and meta-analyses
- National and international treatment guidelines
- Professional bodies and regulatory authorities
- Verified public data from reputable institutions
We do not use anecdotal reports, unverified claims, or commercially biased sources. Every factual claim is supported by established evidence.
Conflicts of Interest
THE BALANCE provides private mental health and addiction treatment services. However, our clinical reviewers ensure that all content remains objective, non-promotional, and balanced. When discussing treatment options, we outline limitations, risks, and alternatives. Our priority is reader safety and informed decision-making.
How to Use This Information Safely
Mental health and addiction conditions are complex and vary significantly between individuals. The information in this article is provided for general educational purposes only and should not replace professional medical advice, diagnosis, or treatment. If you or someone you know is experiencing symptoms, seek guidance from a qualified healthcare professional. To maintain accuracy and trust, THE BALANCE updates articles regularly as new research and clinical guidance become available.
Do you need help?
If you’re struggling, you don’t have to handle it alone. Support is available - whether you’re feeling overwhelmed, anxious, depressed, or dealing with alcohol or drug-related concerns. If you feel unsafe, are at risk of harming yourself, or someone else is in immediate danger, contact your local emergency number immediately.
Talk to Someone Now (Free & Confidential)
Choose your country to find a trusted helpline near you:
Spain
- Suicide & emotional crisis helpline: 024 (24/7, free, multilingual)
- Samaritans in Spain: 900 525 100 (24/7)
Switzerland
- Die Dargebotene Hand / La Main Tendue: 143 (24/7)
- Pro Juventute (youth): 147
United Kingdom
- Samaritans: 116 123 (24/7, free)
- NHS urgent mental health support: call 111 (24/7)
United States
- 988 Suicide & Crisis Lifeline — call, text, or chat 988 (24/7)
Canada
- 9-8-8 Suicide Crisis Helpline — call or text 988 (24/7, nationwide)
- Talk Suicide Canada (alternate): 1-833-456-4566
France
- National suicide prevention number: 3114 (24/7, free)
Germany
- TelefonSeelsorge: 116 123
- Alternate numbers: 0800 111 0 111 / 0800 111 0 222
Italy
- Telefono Amico Italia: 800 860 022 or 02 2327 2327
Not an Emergency, but You Want Support?
If you’re not in immediate danger but are worried about yourself or someone you care about, reaching out early can make a meaningful difference.
Explore Care Options Near You
This website lists verified mental health professionals, addiction specialists, and treatment programs searchable by country and location. Use the “Find treatment” / “Providers” section to explore available options.
Or Reach Out to Us
If you’d like help understanding next steps, you can contact our team confidentially. We’ll listen without judgment and help you explore appropriate options.
Contact our team
- Phone: +41445005111
- Email: help@thebalance.clinic
- Availability: Mon–Sun, 07:00–22:00 CET
Not sure what to say? You can simply write: “I need help.” We’ll take it from there.



